United Healthcare Restricts Insulin Pump Choice
As insurance companies are increasingly maneuvering to restrict patient choices on all types of diabetes devices and medications, the latest move by UnitedHealthcare to make Medtronic its exclusive in-network supplier of insulin pumps has outraged the patient community.
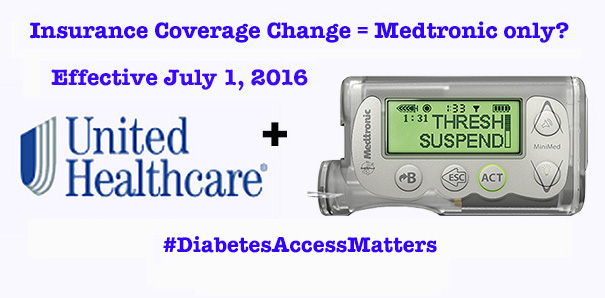
News of this UHC change came in early May 2016, with Tandem Diabetes Care being the first to put out a press release calling attention to the new policy, stating that as of July 1, 2016, adult PWDs (over age 18) covered by UnitedHealthcare will have a much more difficult time obtaining a new, non-Medtronic brand of insulin pump.
What's especially frustrating is that UHC buried the information about this change on Page 7 of a 31-page document sent out recently to doctors and patients. It took an industry competitor to blow the whistle, as it were.
UnitedHealthcare's new Medtronic policy
Here's what you should know:
- This only applies to traditional insulin pumps -- from Animas, Roche and Tandem. It does not apply to Insulet's OmniPod, as the insurer doesn't consider the patch pump part of the standard DME (durable medical equipment) category.
- Supplies for existing in-warranty pumps won't be affected, meaning if you're using an Animas, Roche or Tandem pump, you can still get the needed supplies as long as your pump is still under warranty and not malfunctioning.
- This new rule does not apply to patients 18 and under (likely due to Medtronic not having pediatric approval for its latest 530G pump-CGM combo).
- This change doesn't apply to UHC Sierra Health, Life Commercial, or Medicare Advantage plans.
- Exceptions may be made. The policy states that patients may still be granted coverage for non-MedT pumps on a case-by-case basis, determined by a TBD set of clinical indications that we've yet to see outlined anywhere.
- If granted an exception, the member may be able to obtain a non-Medtronic pump through UHC's in-network distributor, Byram. Or if the member’s plan has out-of-network benefits, they may also obtain the alternate
pump through their out-of-network prover, but may have higher out of pocket costs.
It seems the only way for patients to fight for the pump of their choice is to work with their doctor to show evidence of "clinical criteria" indicating that a pump other than Medtronic is needed.
"These cases will be determined one-on-one with the prescribing physician and if approved would be covered at the in-network benefit level," UHC's corporate communications spokeswoman Kristen Hellmer tells us -- without providing any details on what those clinical criteria may be. (And any of us who've dealt with insurance companies know what a hassle it is trying to nail down what they want!)
For now, this UHC change only applies to insulin pumps -- but it's not difficult to imagine how this could easily be extended to continuous glucose monitors (CGMs), i.e. Medtronic's competitor Dexcom that's also integrated into the Tandem t:slim G4 and Animas Vibe pump systems. And you can see how this could logically progress to closed loop systems, to block competitors to Medtronic's next-gen 670G hybrid closed loop expected sometime in 2017.
It's very likely Medtronic has been pitching its current tech and next-generation system to UHC in coverage negotiations, suggesting that it's more cost-effective to lock patients into a single-vendor setup. The fact is that Medtronic pulls the strings by pitching rebates and better prices to UHC and other insurers, effectively advocating for their system and no other.
The big national diabetes organizations including JDRF, the American Diabetes Association (ADA), the American Association of Diabetes Educators (AADE), and the American Association of Clinical Endocrinologists (AACE) are reviewing this and coordinating responses, along with others in the diabetes device industry.
Many of us have been told by insurers for years that we must use preferred brands of test strips, meters, insulin and other medications. But now, that's moving into the highly-competitive insulin pump market. The really scary thing here is that UHC is essentially setting the stage for other insurers to roll out similar insulin pump restrictions -- crippling the freedom of patient choice that our community has so passionately advocated for.
What UHC says
UHC tells us the two companies will work together to "advance diabetes care" by better tracking clinical outcomes based on Medtronic pump data.
“UnitedHealthcare and Medtronic are working together to better serve people with diabetes by combining their collective resources, data and expertise," Hellmer wrote in an email statement. "This will include assessing how the combination of advanced technologies and patient support programs can improve care plans for individuals using insulin pumps... we aspire to bring a value-based approach to diabetes care that tracks clinical outcomes for UnitedHealthcare members on insulin pumps and places greater focus on quality rather than the volume of care delivered."
We aren't sure exactly what that means, but UHC currently has circa 15,000 insured members nationwide using non-Medtronic pumps -- so sorry Folks, you're actually doing a disservice to at least that many people, just for starters!
We asked UHC point-blank whether they sought any feedback from patients and providers before making this decision, and got only a vague answer that indicates not. "We are continuously engaging with the diabetes community to discuss and learn about ways to improve care and we use that feedback to inform a variety of our initiatives," Hellmer said.
Get ready, UHC. If you want "engagement" from our D-Community, here comes a firestorm!
The Diabetes Community reacts
The Diabetes Online Community (DOC) has lit up over this issue. We first saw the CGM in the Cloud group on Facebook respond, followed by many others on Facebook, Twitter and in the blogosphere.
A handful of hashtags are emerging to capture reactions, mainly #MyPumpChoice and #PatientsOverProfits, as well as #AccessMatters and #PatientVoice. But most recently, it seems #DiabetesAccessMatters is gaining steam to be the main hashtag used to motivate the masses.
Our friend and fellow diabetes advocate Christel Aprigliano penned a remarkable response titled, "How is Milk Like Insulin Pumps?," and other read-worthy statements came from Adam Brown and Kelly Close at diaTribe, Amy Bevan at Glu, Melissa Lee at A Sweet Life, and advocates Kelly Kunik, Pam Osbourne, Stephen Shaul, Kerri Sparling, and Liz Wedward.
The resounding theme: You're screwing with our freedom of choice and access to the best tools, UHC. And that's not OK!

Medtronic & diabetes industry response
When we reached out to Medtronic for their POV, they didn't offer much more than a canned PR statement. With all the criticism heating up, we honestly thought the company would be a little more empathetic about the impact on patients -- especially since they've been pushing a "patient centric" message recently.
Crazy to think that it was just a few weeks ago when they hosted a group of D-advocates for their annual Diabetes Advocates Forum (#MedtronicDAF), chock full of feel-good messages about their commitment to "transforming diabetes care together."
Unfortunately, in its statements, Medtronic only praises its own technology and how this will benefit patients.

Meanwhile, their competition is up in arms.
As noted, Tandem was the first to sound the bell by issuing a press release that brought the issue to light on Tuesday morning.
This quote by Tandem's CEO Kim Blickenstaff says it all: “Having diabetes isn’t a choice. How people manage it should be. Insulin pumps are not a one-size-fits-all solution. Selecting which pump is the best fit for a person to manage their therapy needs to and should be a decision made between a person and their healthcare provider."
Dexcom isn't staying silent on this, either.
"We view this as really not very fair to the patient community," Dexcom CEO Kevin Sayer said in a phone interview. Addressing how Medtronic may try to push this reimbursement advantage beyond insulin pumps into the CGM space, had added: "We will go after this... We're developing a plan of attack, which is not formed yet, given that we just got this news today (May 3) like everyone else."
Others in the pump market and diabetes industry say they're also not happy. Thankfully, the big diabetes orgs -- ADA, AADE, AACE, and JDRF -- have already taken public stances on diabetes device access. We'd like to see them coordinate on this issue specifically and respond en masse, especially given that three of the biggest annual conferences (the AACE, ADA and AADE annual meetings) are coming up quickly, where thousands of diabetes medical folk will gather. This would be the ideal time to hit this issue head-on before and right after the UHC-proposed July 1 start date.
What can we patients do?
We're grateful to our D-advocacy brothers and sisters in arms at diaTribe for leading a charge to activate the patient community on this. They organized an ad hoc conference call with many D-advocates yesterday to come up with several things we in the D-Community can all do immediately. Several dozen diabetes advocates are also collaborating on an open letter to payers about this issue, so stay tuned for more on that soon.
Remember, you don't have to be an UHC insurance customer for this to impact you. It has implications for ALL of us, so please raise your voice and let UHC -- and also your own insurance company -- know that we find this unacceptable!
- Share our stories! We need to hear how this access issue impacts people, and then share those stories with health insurers, diabetes device manufacturers, medical professionals, and elected officials. On Wednesday, the Diabetes Patient Advocacy Coalition (DPAC) created an online hub to facilitate this story-sharing. Visit DPAC's Access Matters to share your own thoughts.
- Reach out to UHC and tell them how you feel. You can reach UHC and its parent group UnitedHealthGroup on Twitter at @myUHC and @AskUHC. Or write a letter or make a phone call to their execs.
- Do the same with Medtronic, letting them know you aren't happy with these exclusive agreements and that you'd like to see them nix any others that may be in the works. Reach them at @MDT_Diabetes or at Facebook.com/MedtronicDiabetes.
- Talk to your diabetes care team about this, too! This insurance mandate on insulin pumps means it becomes more work for you and your medical team to get the device you want. So let's help physicians and educators understand what's happening and encourage them to echo these concerns up the chain.
- Advocate to employers and insurance brokers. Employees with workplace health plans can take their advocacy to insurance brokers, who often have effective channels to communicate back to these payers (insurance companies). If enough employer health plans start raising a fuss about this with UHC and other insurers, maybe they'll rethink any policy change decisions impacting patient choice.
Our D-Community is clearly passionate about freedom of patient choice and unrestricted access to diabetes tools. If we can't choose the best tools for us individually, that's a huge factor in how well we can manage our illness! Which in the end adds cost to the healthcare system.
Listen up UHC and Medtronic: Let us decide for ourselves, instead of forcing our hands and making us spend yet more time and energy fighting to get what we need to lead healthy lives.
- - - - - - - - - - - - - - - -
Originally reported and published at DiabetesMine in May 2016

Comments